EVOLVING ADHD NEUROLOGY
Psychiatric
comorbidities are often linked to ADHD1
Studies have demonstrated neurological as well as emotional dysregulation associated with ADHD.1
Understanding Neurology and Link to Emotional Comorbidities
Children with ADHD frequently experience other psychiatric symptoms beyond core features2
ADHD is one of the most heritable psychiatric disorders with heritability estimates ranging from 60 to 90%3
The pathogenesis of ADHD is complex, involving an interplay of genes and environment2,4,5
Genetics
Genetic factors have shown to contribute to the onset, persistence, and remission of ADHD—and may account, in part, for the co-occurrence of ADHD with emotional dysregulation.1
Environment
Environmental risk factors that interact with genetic and epigenetic vulnerabilities play a significant role in ADHD likelihood, including6-9:
- Poor maternal nutrition, maternal anemia, parental psychopathology and lower socioeconomic status, complicated and/or stressful pregnancy, prematurity and prenatal exposure to drugs (eg, tobacco, cocaine, alcohol, antidepressants) and toxins like lead6-9
“The heterogeneity of [ADHD] is shown by its extensive psychiatric comorbidity… and the wide range of structural and functional brain anomalies."1
-Stephen Faraone, MD, et al
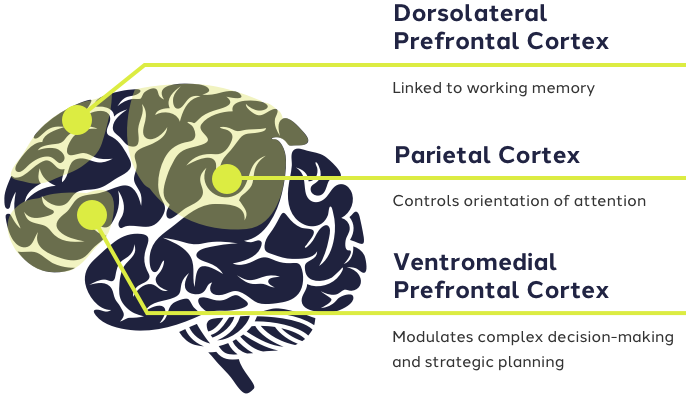
The overlap of psychiatric symptoms points to a dysregulation in the neurologic pathways seen in children with ADHD. In particular, cortical and subcortical regions of the brain are implicated, including the1:
Neurotransmitter circuits are also involved in ADHD and include the1:
Dopaminergic system
Plays a key role in the planning and initiation of motor responses, activation, and reward seeking
Noradrenergic system
Influences arousal and cognitive processing of urgent stimuli
Likewise, executive control networks have also been shown to be underactive in patients with ADHD, leading to deficiencies in planning, goal-directed behavior, inhibition, working memory, and cognitive flexibility.1
In addition to psychiatric comorbidities, certain physical health issues have been shown to correlate to an ADHD diagnosis:
A recent meta-analysis of a large-scale population-based study supports a significant association between asthma and ADHD.10
Dysbiosis of gut microbiome has also recently been shown to predict dopamine precursor synthesis in adolescents with ADHD, leading to decreases in neural reward anticipation.11
For a more detailed look at ADHD, download The Neurobiology of ADHD White Paper
Neurobiology of ADHD: Why ADHD May Predispose Patients to Common Comorbidities
Dr. Maletic, MD, MS, clinical professor of Neuropsychiatry and Behavioral Science at the University of South Carolina School of Medicine in Greenville, SC, discusses the neurobiology of ADHD and the relevance in understanding its relationships with common ADHD comorbidities.
Hello. My name is Vladimir Maletic. I am a clinical professor of Neuropsychiatry and Behavioral Science at the University of South Carolina School of Medicine in Greenville, South Carolina. The topic of this video is the neurobiology of attention-deficit/hyperactivity disorder (ADHD), and the relevance in understanding its relationship with common ADHD comorbidities.
A good place to start our presentation is by reviewing some of the more recent genetic studies. Very large-scale genome-wide association studies comparing the genetic makeup of approximately 20,000 individuals with ADHD to that of approximately 35,000 healthy controls have pointed to some very interesting associations. 1
For example, having a genetic makeup that carries a risk of ADHD is also associated with increased risk of alcohol intake and dependency, depression, mood swings, and feeling miserable, irritable, tense, and high-strung. 1
This raises an interesting question – Are these tendencies towards higher risks of specific emotional behaviors and tendencies toward comorbidities such as substance use and depression actually comorbidities of ADHD? Or are they actually manifestations of the ADHD genetic underpinning itself? Hopefully, further research will offer an answer. 1
To continue our discussion, I will briefly speak about the prefrontal cortical networks that are relevant to ADHD. We can begin by looking at the cognitive-executive network [animate blue text and arrows]. This network comprises interconnected cortical areas that have a role in executive function and working memory, as well as selective and sustained attention. Furthermore, dorsal prefrontal cortical areas participate in “top-down” regulation of emotion. In addition, prefrontal cortical areas are connected to premotor cortices, where they participate in the planning of motoric activity. Individuals who have ADHD have been found to have abnormalities in these connections. 2-5
The next network I want to bring up is the cortico-striatal- thalamic- cortical network [animate purple text and arrows]. This network comprises parallel loops that connect the prefrontal cortex with the basal ganglia and thalamus. The relevance of this network in ADHD is that it has a role in regulating ascending sensory information that reaches the prefrontal cortex and assigning salience to this information, as well as inhibiting inappropriate actions and motivation. 5,6
Finally, connections in the cortico-limbic network [animate red text and arrows] originate from the ventral prefrontal cortex and connect with limbic areas, such as the amygdala and hypothalamus, as well as with brainstem norepinephrine nuclei that regulate the level of arousal. Dysfunction of these connections in ADHD may result in emotional lability, as well as deficits in impulsivity and motivation. 4,7-9
We also know that ADHD is associated with structural changes in the dorsolateral prefrontal cortex (DLPFC) and the anterior cingulate Cortex (ACC). The images I am going to show you are from an MRI study that compared 24 adults with ADHD with 18 healthy controls.Blue coloring indicates a decrease in volume, and red coloring indicates an increase in brain volume compared to normal brains. 10-12
As we can see in these images, those with ADHD had an increased volume in white matter and a decreased volume in grey matter, including decreases in the volume of the dorsolateral prefrontal cortex and cingulate [animate the labels, “DLPFC” and “CGa”]. 10
These are some of the most replicated findings in ADHD. What may be potential implications of these findings for ADHD? As noted previously, these areas have a key role in the so-called top-down regulation of emotion. But, in addition to emotional regulation, they’re also hubs of the cognitive-executive network, so they have a pivotal role in regulation of attention and executive function. 2,10-11
Other functional imaging studies have also noted additional interesting differences between individuals who have ADHD and those who do not. For example, when ADHD subjects and controls, while undergoing functional imaging, observe photographs of strong emotional expressions (such as fear vs neutral expressions), they will have different emotional responses that coincide with changes in activation of relevant limbic areas. 12
Unmedicated individuals with ADHD have more intense responses in their amygdala compared to healthy participants. 12
If individuals with ADHD are treated with medication, their subsequent imaging reflects normalization of the limbic area responses to emotional stimuli. What is interesting is that these stimuli are so brief that they are not consciously registered, but nonetheless, brain responses to these stimuli can be readily observed on the MRI. 12
Moving on from findings regarding limbic structure responsivity, let’s shift our focus to the role of basal ganglia in ADHD. As I mentioned previously, the basal ganglia are part of the cortico-striatal-thalamo- cortical pathways and are involved in motivation, as well as suppression of hyperactivity and impulsivity. As seen here, structural studies have noted smaller volumes of the ventral striatum in individuals with ADHD compared to controls. 5,6,13
In addition, the globus pallidus, caudate, thalamus, and putamen have lower volumes in patients with ADHD, again possibly indicating a relationship with hyperactivity and impulsivity. 14-16
Not only does the genetic underpinning of ADHD predispose individuals toward ADHD-associated symptomatology, functional and structural imaging findings provide evidence of corresponding brain changes that would reflect these phenomena. This brings up the question of whether there are any abnormalities in neurotransmission and the neurotransmitter pathways that innervate these particular cortical and limbic areas. For several decades, the focus has been on norepinephrine and dopamine transmission. We find that norepinephrine pathways originating from the locus coeruleus richly innervate prefrontal cortical areas, as well as limbic areas. The question is, is there any abnormality in norepinephrine and dopamine transmission in individuals suffering from ADHD? 17-19
As this graphic illustrates, there appears to be an inverted U-shaped and delicate balance in the relationship between influx of norepinephrine and dopamine and prefrontal cortical function. 20
If there is too little norepinephrine and dopamine flowing to the prefrontal cortex, individuals are likely to be distracted or disorganized, forgetful, and impulsive. 20
If norepinephrine and dopamine input is optimal, these neurotransmitters will bind to the receptors that have a high affinity for norepinephrine and dopamine. Optimal transmission will be reflected in wakefulness, alertness, good attention, executive function, and working memory. 20-23
On the other hand, if dopamine and norepinephrine input is excessive (as may be the case in extremely stressful situations or with an excessive stimulant dose), they will bind to the receptors for which they have lower affinity or that have an extrasynaptic location. Rather than being focused, individuals now become distracted, and they may be anxious (sometimes on the verge of panic attack), irritable, and may have difficulty falling asleep. 20,24
In summary, ADHD is a very complex condition. Most likely, it is not a singular biological entity, but rather it represents several different biotypes that have similar manifestations. Genetic studies suggest that ADHD is an extreme expression of continuous heritable traits. The genetics of ADHD suggest that many of the traits related to emotional responses, anxiety, and possibly even substance use may be part and parcel of the genetics of ADHD, as well as its common comorbidities. 1-2,5,
Furthermore, ADHD is associated with both structural and functional brain changes involving areas that participate in regulation of attention, working memory, and executive function, as well as top-down regulation of emotion. Neurotransmitters that are most involved in the pathophysiology of ADHD include dopamine and norepinephrine, although newer studies have also implicated GABA and glutamate. 3-5,25-30
Finally, suggesting that ADHD and some of its common comorbidities have shared genetics and functional and structural involvement raises some questions; mainly, since ADHD itself has a propensity toward anxiety, mood dysregulation, and vulnerability toward substance abuse, are these manifestations of ADHD or truly comorbid conditions? 25-30
Thank you very much for your kind attention and for being part of the TEAM ADHD educational initiative.
REFERENCES: 1. Du Rietz E et al. Biol Psychiatry Cogn Neurosci Neuroimaging. 2018;3(7):635-643. 2. Bressler SL et al. Trends Cogn Sci. 2010;14(6): 277-290. 3. Smith SD et al. Brain Connect. 2019;9(6):508-518. 4. Comte M et al. Cereb Cortex. 2016;26(1):144-155. 5. Arnsten AF et al. J Am Acad Child Adolesc Psychiatry. 2012;51(4):356-367. 6. Peters SK et al. Front Syst Neurosci. 2016;10:104. 7. Gunnar M et al. Annu Rev Psychol. 2007. 58:145-173. 8. Gupta A et al. J Neurosci Res. 2017; 95(9):1760-1775. 9. Gehricke JG et al. PLoS One. 2017;12(4):e0175433. 10. Seidman LJ et al. Biol Psychiatry. 2006;60(10):1071-1080. 11. Petrovic P et al. Behav Neurosci. 2016;10(70):1-25. 12. Posner J et al. J Am Acad Child Adolesc Psychiatry. 2011;50(8):828-837. 13.Soliva JC et al. Ann N Y Acad Sci. 2009;1167:212-220. 14. Nakao T et al. Am J Psychiatry. 2011;168(11);1154-1163. 15. Ellison-Wright I et al. BMC Psychiatry. 2008;8:51. 16. Collins AM. J Nurse Pract. 2014;10(1):16- 21. 17. Kollins SH, Adcock RA. Prog Neuropsychopharmacol Biol Psychiatry. 2014;52:70-78. 18. Glaser PEA et al. The neuropsychopharmacology of stimulants: Dopamine and ADHD, current directions in ADHD and its treatment. Jill M. Norvilitis (Ed.), ISBN: 978-953-307-868-7, InTech, http://www.intechopen.com/books/ curren t-directions-in-adhd-and-its-treatment/ theneuropsychopharmacology-of- stimulants-dopamine-and-adhd. 19. Sara SJ, Bouret S. Neuron. 2012;76(1): 130-141. 20. Arnsten AFT. CNS Drugs. 2009;23(suppl 1):33-41. 21. Berridge CW, Spencer RC. Brain Res. 2016;1641(Pt B):189-96. 22. Watson CJ et al. Sleep Med Clin. 2010;5(4):513-528. 23. Logue SF et al. Pharmacol Biochem Behav. 2014;123:45-54. 24. Yamamoto K et al. Psychiatry Clin Neurosci. 2014;68(1):1-20. 25. Faraone SV et al. Nat Rev Dis Primers. 2015;1:15020. 26. Barth B et al. Psychiatry Clin Neurosci. 2018;72(11):836-848. 28. Owen MJ et al. World Psychiatry. 2017;16(3):227-235. 29. Arnsten AF. CNS Drugs. 2009;23(suppl 1):33-41. 30. Purkayastha P et al. Curr Med Chem.2015;22(15):1850-1859. 31. Kooij JJ. J Atten Disord. 2012; 16(5):3S- 19S.
Key Takeaways
- The pathogenesis of ADHD is complex2,4,5
- Dysregulation in the neurologic pathways is seen in children with ADHD1
Stay in the know and access an exclusive ADHD resource
“Unmasking ADHD” can help you differentiate between ADHD and the most common overlapping comorbidities in children.
UP NEXT:
REFERENCES
- Faraone SV, Asherson P, Banaschewski T, et al. Attention-deficit/hyperactivity disorder. Nat Rev Dis Primers. 2015;1:1-23.
- Banaschewski T, Becker K, Dopfner M, Holtmann M, Rosler M, Romanos M. Attention-deficit/hyperactivity disorder. Dtsch Arztebl Int. 2017;114(9):149-159.
- Thaper A. Discoveries on the Genetics of ADHD in the 21st Century: New Findings and Their Implications. Am J Psychiatry. 2018;175:943-950.
- Acosta MT, Arcos-Burgos M, Muenke M. Attention deficit/hyperactivity disorder (ADHD): complex phenotype, simple genotype? Genet Med. 2004;6(1):1-15.
- Shadrin AA, Smeland OB, Zayats T, et al. Novel loci associated with attention-deficit/hyperactivity disorder are revealed by leveraging polygenic overlap with educational attainment. J Am Acad Child Adolesc Psychiatry. 2018;57(2):86-95.
- Minzenberg MJ. Pharmacotherapy for attention-deficit/hyperactivity disorder: from cells to circuits. Neurotherapeutics. 2012;9(3):610-621.
- Cortese S. The neurobiology and genetics of Attention-Deficit/Hyperactivity Disorder (ADHD): what every clinician should know. Eur J Paediatr Neurol.2012;16(5):422-433.
- StergiakouliE, Thapar A. Fitting the pieces together: current research on the genetic basis of attention-deficit/hyperactivity disorder (ADHD).Neuropsychiatr Dis Treat.2010;6:551-560.
- Clements CC, Castro VM, Blumenthal SR, et al. Prenatal antidepressant exposure is associated with risk for attention-deficit hyperactivity disorder but not autism spectrum disorder in a large health system. Mol Psychiatry.2015;20(6):727-734.
- Cortese S, Sun S, Sharma E, et al. Association between attention-deficit/hyperactivity disorder and asthma: a systematic review and meta-analysis and a Swedish population-based study. Lancet Psych. 2018;5(9):P717-P726.
- Aarts E, Ederveen THA, Naaijen J, et al. Gut microbiome in ADHD and its relation to neural reward anticipation. PLoS One. 2017;12(9):e0183509.